Living with pain isn’t something anyone should have to endure, but sometimes it’s a fact of life. Oftentimes one is forced to lay in bed for long periods of time, and pressure ulcers and sores, otherwise known as bedsores, can develop.
Fortunately, there are special kinds of bedding which can be used to help avoid the development of these issues, but not all are created equal. There are certain things to consider when looking to purchase exactly what you need to keep yourself, or someone you love, free from these awful issues.
1. What are Pressure Ulcers?
The term “bedsore” is one you’ve likely heard many times over the years. I know I certainly had. Until recently, though, I didn’t really know what a bedsore was. I figured it was something which only struck the elderly for one reason or another. On the contrary, anyone can fall victim if the right conditions are met.
Bedsores, more specifically pressure ulcers or pressure sores, typically result from pressure which is placed on a specific part of the skin for a long period of time, typically over some sort of protrusion, such as a bone. Such is the case with people who are bedridden for long periods of time, or who have to constantly be sitting. Anyone forced to be in these positions is at risk, from a healthy person in a wheelchair to a comatose person in a hospital bed.
2. Causes
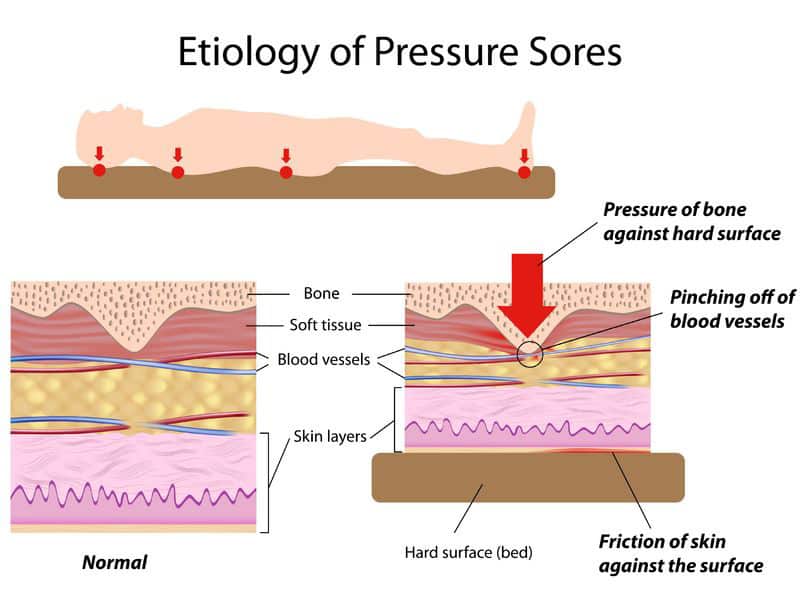
When it comes to bedsores, there are two primary factors involved: pressure and friction. Together, these two work to cause the skin to tear, resulting in the beginnings of a pressure ulcer. It starts simply enough, but can advance quickly.
First, pressure is exerted on a single part of the body. In many cases, the first place is often the sacrum and the coccyx, which are the bone just above the tailbone, and the tailbone itself. In this early stage, pressure occurs when the skin is pushed against the bones for long periods of time.
Then, as time passes, friction begins to happen as the body shifts and adjusts little by little, causing damage to happen to the blood vessels which lay just beneath the surface of the skin. Any time the body is moved, whether it be from shifting or from being adjusted, that friction can occur, further exacerbating the issue.
Finally, after the skin has been made sensitive and weak from friction, a shear can occur. This is when the skin pulls away from the muscle and such below the skin. Oftentimes this happens when the skin sticks to a bedsheet when sitting up or adjusting.
Once the process is complete, the skin has become weak enough to allow for it to tear and open up, creating the perfect conditions for infection due to external factors such as the presence of fecal matter or other materials which may exist in unsanitary situations. Bacteria positively loves necrotic tissue, and that’s what is left behind when a pressure ulcer is allowed to grow to completion.
3. Stages
There is an organization which oversees the treatment and classification of pressure ulcers in the United States, the National Pressure Ulcer Advisor Panel, also known as NPUAP. NPUAP has set specific guidelines as to the stages a pressure ulcer goes through in order to better guide treatment. These are revised from time to time.
Currently, there are four stages in the cycle of a pressure ulcer, with two additional classifications.
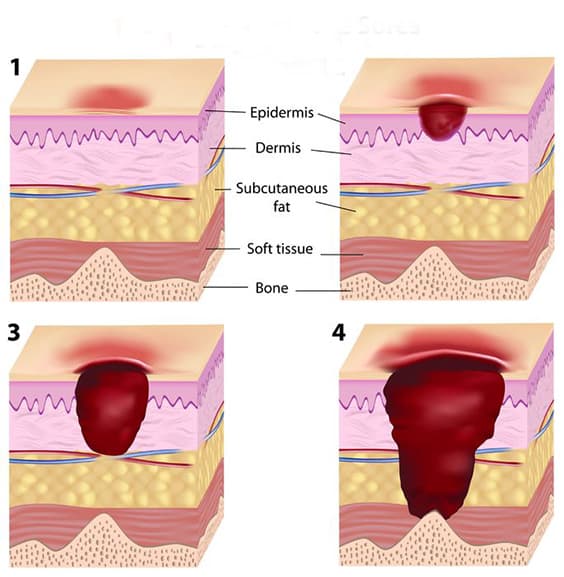
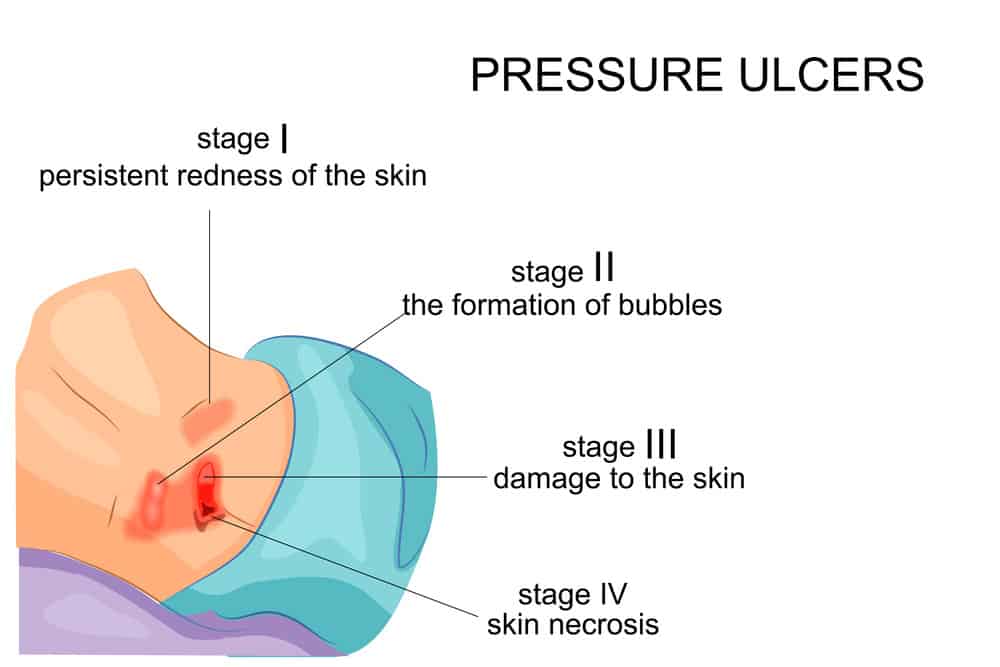
Stage I:
A Stage I pressure ulcer is skin which hasn’t yet torn, but has begun to appear red in a localized area on the skin, typically over a protrusion of bone. The skin will also feel different, but in temperature and in thickness. Since part of detecting this phase is to look for visual cues, diagnosing this stage in people with darker skin tones can be an issue, as the change in color may not be as apparent.
Stage II:
In Stage II cases, the skin has begun to thin out and the area turns a brighter red. In some cases, Stage II also presents as a blister. There are several unrelated conditions which can show similar symptoms and should not be confused. These include skin tears, tape burns and other issues related to the skin.
Stage III:
By the time a pressure ulcer hits Stage III, things have gotten pretty bad. The top level of the skin will likely have fallen away and the ulcer will be exposed, sometimes even revealing the fat which exists under the skin. In this stage, bone and other underlying tissue are not yet visible. Depending on where on the body the bedsore is appearing, a Stage III pressure ulcer can have a varying thickness. Sections of the body with more fat content are more likely to have deeper Stage III ulcers than those without.
Stage IV:
As with a Stage III pressure ulcer, Stage IV can have varying depths, but it will always mean the skin has pretty much gone away completely. With a Stage IV pressure ulcer, whatever was lying beneath the skin is now exposed. This can be bone, tendon, cartilage or muscle, depending on the location of the pressure ulcer. Because it has become exposed, an infection of the bone, called osteomyelitis, has a high risk of happening.
Unstageable:
When a pressure ulcer still has intact dead skin above it, its depth and severity can be difficult to discern. At this point, it is considered Unstageable. In order to properly classify an Unstageable bedsore, the skin needs to be removed so the level of damage can be determined and treatment can begin. In some cases, however, the skin should not be removed, as it can sometimes continue to serve in a protective fashion. This varies depending on where on the body the sore exists.
Suspected Deep Tissue Injury:
One stage isn’t quite a stage, so much as a warning sign. When the skin develops a purple or maroon tone in a localized area which has remained intact, it can sometimes be an indication of deeper issues to the underlying tissue. With a deep tissue injury, pressure ulcers can progress very quickly, even with ideal levels of treatment.
4. Treatment
Since one of the primary issues with pressure ulcers is dealing with skin and tissue which has died, some cautions must be taken when the treatment phase begins. Additionally, treatment can vary to some extent depending on the severity of the damage and on which stage the pressure ulcer exists.
The first step is the removal of any dead tissue which exists within or around the bedsore. This can be a harrowing process, but a necessary one. Bacteria love necrotic tissue, so infection is highly possible and healing becomes very difficult. Removing the necrotic tissue is vital to healing. There are five methods which can be used to remove the necrotic tissue.
The first involves the stimulation of the immune system to do the work itself. Moist dressings can be placed on wounds to help encourage the creation of white blood cells and enzymes which can break down the necrotic tissue and promote healing. It takes longer than other methods, but doesn’t cause any major pain. This doesn’t work in those with poor immune systems, however.
Another method is far more gruesome, involving some external biological help. A process called biological debridement involves introducing maggots to the wound and allowing them to eat the dead tissue, and the bacteria with it. This may sound like something from the dark ages of medicine, but it is an FDA approved procedure as of 2004.
Chemical debridement introduces enzymes the body isn’t producing which can help cause the necrotic tissue to begin to fade away.
Mechanical debridement is simply the use of some sort of external tool to help get rid of the dead tissue. This can be special dressings, a whirlpool or even an ultrasound. Each of these can help slough off those dead cells in order to begin promoting the growth of new ones.
The fastest way to get the necrotic skin out of there is surgical debridement, which is exactly what it sounds like. A surgeon gets in there with a scalpel and cuts the stuff out. It’s quick and moderately painless, but is also the least natural of all of the procedures.
Additionally, the NPUAP has put into place guidelines involving the dressing of pressure ulcers in order to encourage healing. Bedsores which are leaking very little fluid can simple use gauze with tape, while those with heavy amounts of exudates should use a foam dressing.
If the subject is at risk of frequent soiling, a hydrocolloid dressing, film or composite should be used in order to keep the area clean.
In the case of very fragile skin, such as with an elderly person, stretch gauze or stretch net can be used in order to keep the skin from becoming further damaged due to stresses caused by gauze and such which has no give.
These methods and guidelines are, as of this time, the best ways to not only begin proper treatment of a pressure ulcer, but ways to keep them clean and free from infection, and hopefully to keep them from showing up again.
5. Prevention
Several methods can be used in order to prevent, or at least slow, the development of pressure ulcers in patients. Guidelines created by the NPUAP and its European counterpart, EPUAP, have worked to extend and enhance the lives of many who have suffered from bedsores.
Since these issues don’t develop without pressure, hence the name pressure ulcers, one of the most important things you can do to help combat bedsores is to adjust and redistribute pressure. In hospitals, where people can often go long times without ever getting out of bed, redistributing pressure is of utmost importance. The procedure typically involves turning the patient, and then using support surfaces to move the largest pressure points to other sections of the body.
For instance, simply lying on the bed puts pressure onto the sacrum and coccyx, but by using special support pillows and such, the largest pressure can be moved to, say, just behind the thighs, with the other parts being slightly elevated. When this is done on a regular basis, every couple hours or so, great results can be seen. When this was introduced in the 1940s, the life expectancy of paraplegics in the hospital increased from only two years, as previously they would often die from infections.
Proper nutrition is vital in combating pressure ulcers. In bedridden patients, it has been proven that people who consume larger amounts of vitamin C actually experience fewer bedsores. The same can be said for newborns who may develop pressure ulcers. Proper nutrition can help strengthen the immune system and help fight off any infections which may occur as a result of a bedsore.
The introduction of new support surfaces has also made its way into the guidelines put forth by the NPUAP. Memory foam mattresses have made the list, as well as special mattresses which have either alternating pressure levels or the ability to redistribute pressure using air pumps. We’ll take a deeper look at the sleep options in our next section.
6. Sleeping with Pressure Sores
Developing pressure sores after being bedridden, or trying to take care of a loved one who may have developed them while spending time in a hospital can be a trying experience. They are quite painful and need to be cared for properly in order to make sure they are healing the right way. They can also greatly interrupt our sleep cycle, but there are tools out there which can help return a restful night’s sleep to those suffering from pressure ulcers.
7. Mattresses
If you’re willing to spend the money, you can absolutely purchase a hospital-grade air mattress which provides alternating levels of pressure and can help turn and adjust the sleeper in order to avoid the development of pressure ulcers. These pressure relieving mattresses don’t typically come in very large sizes, seemingly relegated to only the size of a hospital bed. Still, such a mattress can be a great boon to anyone who is stuck in a bed for most of the time.
For a more conventional option, high-density memory foam mattresses can be a good option. Numbers collected in 2015 showed that those who slept on memory foam of a very high quality were less likely to develop new pressure sores by nearly 60 percent. Because memory foam is able to envelop its sleeper and, basically, distribute pressure all around the body, it does a fair job of helping to make sure no single part of the body has too much. For this reason, a memory foam mattress is a great mattress for bedsores.
8. Pillows and Cushions
Sometimes maintaining a position for extended periods of time can be difficult. Simply lying on your back is the easiest of all options, but this is why pressure ulcers tend to develop in those lower back areas first. Using special pillows and cushions, however, you can help combat the onset of pressure sores, or the exacerbation of new ones, without the need of a special decubitus mattress.
These pillows and cushions come in all shapes and sizes and are made of various different types of material. A triangular cushion can help keep you on your side, and if it’s filled with a gel foam material, it can keep you cooler while making sure you can maintain your new position.
Pillows also exist which can be placed under you when you sit, in case you can’t often get up and move around. Some are just great cushions which redistribute pressure, others still can remove pressure entirely, as with a pillow for those who suffer from hemorrhoidal issues.
9. Extras
Don’t feel your options are limited just because you can’t afford to get a hospital bed or a high quality memory foam mattress. There are a great many options out there which can complement your current setup without breaking the bank. In fact, some of these options may even be your best bet, as they allow you to modify what you’ve already got, while still giving you the freedom to remove them once the issues have subsided.
Mattress toppers are likely some of the best tools for fighting pressure ulcers. You can find them in various varieties, including foam which is several inches thick. This foam can be somewhat successful when it comes to transforming an old innerspring mattress into something a bit more modern. Additionally, air mattress toppers are a great option since they allow for adjustment, just a hospital bed might. Some on the higher end can even offer some of the same options those hospital beds do, and all you have to do is install it by placing it on top of your current mattress, plugging it in and fiddling around with the settings. Real the manual first.
10. Sleep Tips
Let’s be honest, going to sleep while you’re in pain is never an easy thing to do, but there are ways to make it a little easier, at least. Creating the right environment for rest is important, but for someone who is bedridden, many of the usual sleep tip rules have to be thrown out the window.
Tip 1:
Common sleep tips tell you to keep electronic devices, such as televisions and smartphones, out of the room or out of reach. Doing this, however, would certainly drive me mad were I ordered to stay in bed for long periods of time.
Tip 2:
Other tips, however, still hold true. Setting a routine can be important when it comes to preparing your body for actual sleep. Try to fall asleep at the same time every day. Have a cup of caffeine-free herbal tea just before sleeping. Try to read a book or some other form of low-impact entertainment. Incorporating these things will help you body know, by the time you finish that cup of tea, that the next step in your routine is to fall asleep.
Tip 3:
Also, things should be avoided which can interrupt sleep. Spicy foods, for instance, can cause acid build up which can lead to late night issues with heartburn or acid reflux. Chocolate isn’t always a great idea as it can add caffeine to the system, which isn’t good for anyone trying to quickly fall asleep.
Tip 4:
Obviously, large amounts of pain and discomfort can undo anything you might attempt, but getting into the mindset, and putting your body into a calm state of being, can surely assist in you finally falling asleep.
Solutions Exist
You are not alone. For generations, people have had to deal with bedsores, or have had to help those who have. They’re nothing to laugh about, for sure, but they are also incredibly common and can be dealt with using a little bit of care and ingenuity. Thanks to modern tools, this has become much easier, though pressure ulcers haven’t been eliminated entirely.
The key is to keep an eye out for those earlier symptoms. If a pressure sore can be caught in the earliest stages, the preventative measures we’ve discussed can help the body naturally fight back against the friction and pressure which have caused the sores to develop.
Always consult with a healthcare professional regarding these issues, as well. If you’re taking care of a bedridden relative and see what appear to be bedsores forming, don’t just make the decision yourself to help them out. Pick up the phone and make an appointment to have them seen by a doctor. It can be the difference between life and death in cases.
There may be some embarrassment, and perhaps guilt, that you the pressure ulcers were allowed to develop, but there shouldn’t be. A pressure ulcer can happen to anyone, and it isn’t a death sentence as it may have been back in the darker ages of medicine. With the right kind of care and a watchful and loving eye, anyone can recover from a bedsore.